Scientific solutions for the gap in translational medicine: skin model platform with melanoma (3D melanoma)
The developing process of a new drug, from first testing to regulatory approval and ultimately to market is a long, costly, and risky path. Noteworthy is the fact that almost 95% of the drugs that go into human trials fail. According to the National Institutes of Health (NIH), 80 to 90% of drug research projects fail before they ever get tested in humans. The value of preclinical research, mainly conducted in animal model experiments for predicting the effectiveness of therapies and treatment strategies in human trials, has remained controversial. Only 6% of the animal studies are successfully translated into the human response. Breaking down failure rates by therapeutic area, oncology disorders account for 30% of all failures. The absence of human-relevant models with receptors, proteins, and drug interactions in the in situ microenvironment leaves a gap in the scientific discovery process of new therapies. In this context, the present work presents the development of a sophisticated in vitro skin model platform focus on boosting melanoma treatment. The results showed a physiological microenvironment of human skin with epidermal differentiation and development of stratified layers (basement membrane, stratum spinosum, stratum granulosum, and stratum corneum). Furthermore, it was observed the pathophysiological microenvironment of the melanoma with invasion or migration through the basement membrane into the dermis and no epidermal differentiation. Vemurafenib treatment, the gold standard which targets BRAF mutations, showed a decrease in proliferation and invasion of melanoma tumors, with an increase in epidermis keratinization. Melanoma incidence continues to increase year-on-year and is currently responsible for >80% of skin cancer deaths. It is the most common cutaneous form and is known to have the highest mutational load of all cancers. Nowadays, patients with advanced melanoma BRAFV600E mutation can benefit from monotherapies or targeted therapies. Although the initial response rate is effective, disease progression and tumor chemoresistance rapidly occur in the majority of patients. Therefore, the treatment of melanoma remains a challenge, and despite the advances, there is still an urgent need to identify new therapeutic strategies. 3D Model Melanoma is considered one important tool for studying the evolution of the pathology, as well
as evaluating the effectiveness of new therapeutic approaches.
New

Five simple tricks for making your own video for TPI.tv
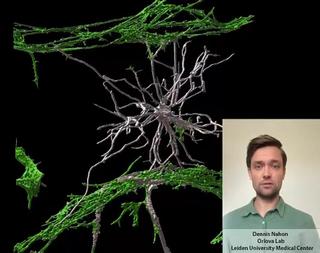
Stem cell derived Vessels-on-Chip to study brain disorders

From 2D hiPSC culture to developing a 3D vessel-on-chip
